Atopic Dermatitis is a non-contagious, extremely common skin disease that affects up to 10-20% of children globally and 2-5% of adults. It is a chronic condition, meaning symptoms can be long-lasting, although babies and children can ‘grow out’ of the symptoms. Typically sufferers experience two phases of the disease – a non-active (“interval”) phase and a more acute active (“flare-up”) phase. For both phases, a good skin care can help alleviate the discomfort.
Signs & Symptoms
What is atopic dermatitis?
Atopic Dermatitis (or Atopic Eczema) is an increasingly common skin disease that affects many adults, children and babies globally. Children are most prone with 90% of sufferers developing Atopic Dermatitis before the age of five and many children do grow out of the disease. It rarely starts in adulthood.

Symptoms appear on the scalp (cradle cap), face and body although the appearance and areas affected differ between babies, children and adults:
- Babies can develop symptoms as young as 2-3 months. A rash usually appears suddenly making skin dry, scaly and itchy. In flare-up phases, infected skin may ooze fluid. Typically babies get Atopic Dermatitis on their face – particularly the cheeks - and scalp (also known as ‘cradle cap’), the knees and elbows. It is very rare for babies to develop atopic skin in the nappy area. Although nappy rash may look similar, it is too moist an area for Atopic Dermatitis to develop.
- Children who develop the disease later in life (between the ages of two and puberty) usually start with a rash on the body which is dry with itchy, scaly patches. Skin tends to be bumpy, thickened and leathery. Common areas affected are the creases of the elbows or knees, neck, wrists, ankles and/or the creases between the buttocks and legs. Symptoms of Atopic dermatitis in children present on the inside of joints (elbows, wrists, behind the knees) as well as the opposed side of the joints such as the point of the elbow or on kneecaps
- Adult Atopic Dermatitis is typified by very dry, scaly skin and a non-stop itch on the face and body.

Atopic Dermatitis typically has two “phases”. During an inactive (or “interval”) phase skin is very dry, irritable and flaky and needs to be moisturised on a daily basis. Active phases (or “flare-ups”) are more demanding and need to be treated with topical medications to calm inflamed skin and alleviate itching.
The disease can be very distressing, not just for the affected children but for their parents too as it can be difficult to stop children from scratching. Children - babies and toddlers in particular - sometimes rub their bodies against their bed clothes, carpets or other surfaces to remove the itch and this can lead to skin infection. This can result in problems with sleep, causing further stress for parents.
That said, effective treatment and good skin care can alleviate much of the discomfort.
How do I know if my child is experiencing a flare-up on their body?
Your child might have a flare-up if…
They have moderate to intense itching.
Their skin is inflamed and sore.
Their skin is weeping fluid and maybe even bleeding.
Your child may not have a flare-up if…
The application of moisturiser alleviates their symptoms.
They are managing to deal with their symptoms without scratching.
Their skin is intact and only slightly flaky.
Attention
If you are unsure about your child’s symptoms seek the advice of a dermatologist.
Read more about children’s skin.
Causes & Triggers
Potential causes and triggers of Atopic Dermatitis on children´s skin
Dermatologists have identified several causative and contributory factors, such as:


- Associations with hay fever and asthma. There is evidence to show that Atopic Dermatitis is linked with both hay fever and asthma. The so-called “atopic march” typically starts with childhood atopic dermatitis and later, during adolescence and adulthood, hay fever and asthma develop.
- Genetic links. If one or more family members has Atopic Dermatitis, their children will be at risk of these three atopic diseases.
- Environment. Children from developed countries, living in urban areas where the intensity of pollutants is higher, and those living in a cold climates are more likely to develop Atopic Dermatitis. In one study, Jamaican children living in London were found to be twice as likely to develop Atopic Dermatitis as those living in Jamaica.
- Gender. Females are slightly more likely to get the disease than males.
- Age of mother at time of childbirth. There is evidence to show that babies born in the later stages of a mother’s child-bearing years have a higher propensity to Atopic Dermatitis.
Sufferers are known to have a deficiency of natural moisturising factors (such as urea and amino acids) and disturbance of the epidermal lipid metabolism. This explains why their skin is more likely to be dry with a disturbed barrier function.
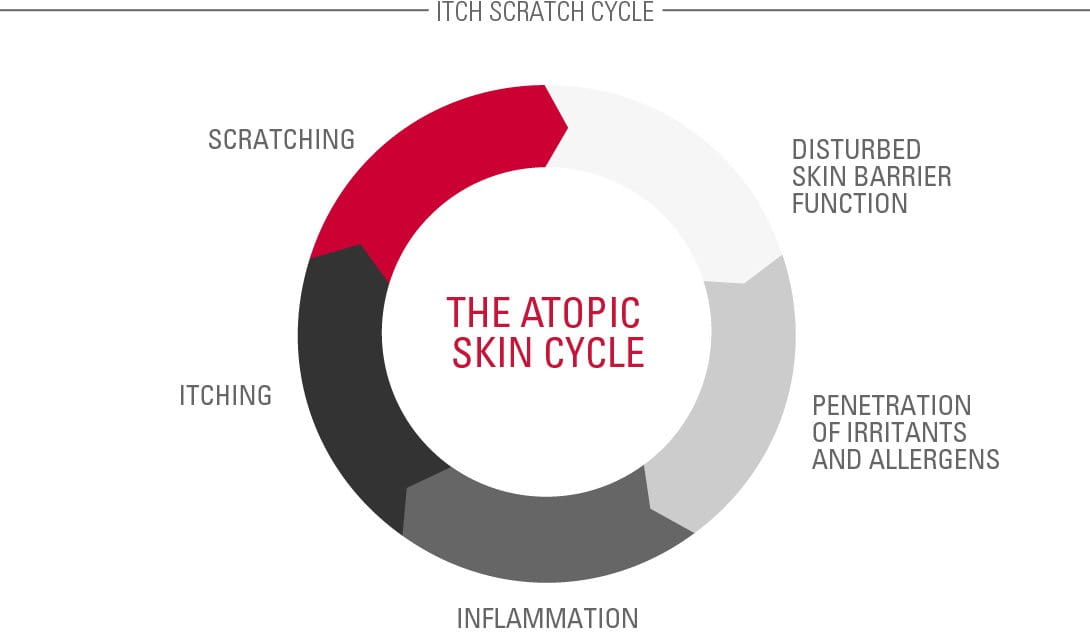
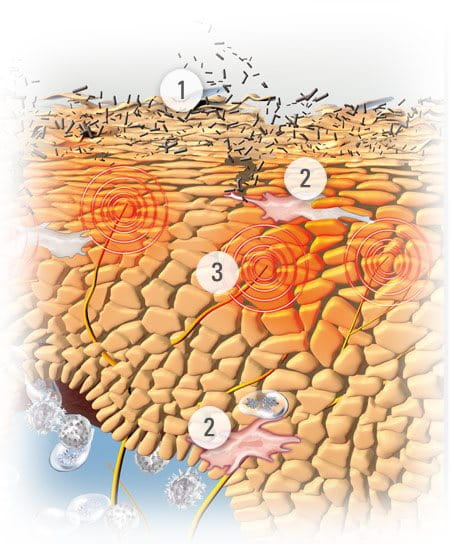
Flare-ups often develop in an Atopic Skin Cycle (see illustration). This is a circle of cause and effect that begins when a child scratches an itch and disturbs their already fragile skin barrier. The exposed layers then become an ideal breeding ground for a bacteria called Staphylococcus aureus. They multiply and infect the skin. The infection causes inflammation, which causes itching, and the cycle starts all over again.
Dermatological treatments help to break the Atopic Skin Cycle.
contributing factors
further contributing factors
Triggers vary from person to person so it can be useful to keep a diary which monitors external factors and their influence on a child’s skin condition. These factors could include:

- Materials that touch their skin, such as nylon (which can cause sweating) and wool (which is an aggravator).
- Foods and drinks. Common examples include milk products, nuts and shellfish. It is important to consult your doctor, however, before you eradicate these from your child’s diet to ensure they don’t miss out on important nutrition).
- Allergies to pet fur, pollen or house mites.
- Psychological stress
- Washing detergents, in particular biological ones.
- Passive cigarette smoke.
- Lack of sleep and stress (side effects of the disease) can both make symptoms worse.
Read more about factors that influence skin.
Solutions
Managing the discomfort of Atopic Dermatitis on children’s skin

Although there is still no known cure for Atopic Dermatitis, all medical therapies recommend consistent application of moisturiser to relieve skin dryness, irritation and itch and reduce emotional stress for both the child and parents.
During an interval phase it is vital to maintain a daily skin care routine, using emollients.
Emollients
Emollients – also known as moisturisers – include creams, lotions and face creams, which can be used together with bath additives and shower oils to maintain skin’s hydration. Supple skin is less itchy so less prone to scratching and irritation.
Key ingredients in the formulas of emollients can include:
- Omega 6 fatty acids. Evening Primrose Oil and Grape Seed Oil soothe and nourish diseased skin and replenish its natural protective barrier.
- Licochalcone A Derived from the licorice root, this is a natural and powerful anti-inflammatory and anti-oxidant which is effective at reducing redness and soothing inflammation.
Dermatological treatments
When flare-ups do occur it is important to supplement emollients with a doctor`s prescription of active care treatments such as medicated creams. These topical creams usually contain corticosteroids.
Corticosteroids are effective and fast-acting ingredients which alleviate the itching of flare-ups almost instantly. However, their application has to be limited according to doctor`s advice.

Eucerin’s AtoControl Acute Care Cream has skin caring properties that have been clinically proven to significantly improve the skin‘s appearance during flare-up phases. This caring skin solution helps reduce the use of hydrocortisone during flare-ups. AtoControl Acute Care Cream is not a pharmaceutical product and is not meant to replace one.
Eucerin AtoControl Anti-Itch Care Spray is an instant relief spray, used in addition to Eucerin AtoControl Acute Care Cream which is useful when out and about. It can be used on children over the age of three years.
Further advice for parents with children with Atopic Dermatitis on the body


- Bathe your child in warm, but not hot, water.
- Restrict bath time to 5 to 10 minutes.
- Do not use bubble bath.
- With babies for the age of three months plus use Eucerin AtoControl Bath & Shower Oil 20% Omega for gentle cleansing relief from irritated skin.
- Pat skin almost dry, then apply emollient straight away.
- Apply emollient at least twice a day.
- Keep fingernails short and smooth so the child cannot scratch and puncture the skin.
- Put cotton gloves on the child at night to prevent scratching in their sleep.
- Keep room temperatures cool and humidity low.
- It can be a good idea to give a child a doll to scratch as this can reduce their need to scratch their own skin.
Our brand values

We deliver a holistic dermo-cosmetic approach to protect your skin, keep it healthy and radiant.

We work together with leading dermatologist and pharmacist partners around the world to create innovative and effective skincare products they can trust and recommend.

For over 100 years, we have dedicated ourselves to researching and innovating in the field of skin science. We believe in creating active ingredients and soothing formulas with high tolerability that work to help you live your life better each day.




