Atopic Dermatitis is a chronic skin disease that is on the increase, particularly in the Western world. It predominantly affects babies and children – as many as 10-20% of children globally – but between 2-5% of adults are also affected. Sufferers have constantly dry, irritable skin which is prone to infection and inflammation. Although there is no known cure, regular skin care - alone or in combination with medical treatments - can alleviate much of the discomfort.
Signs & Symptoms
What is Atopic Dermatitis?
Atopic Dermatitis, which is also known as Atopic Eczema, is a non-contagious chronic skin disease that affects the skin on the face and body of babies, children, and adults. It is on the increase with a two- to three-fold increase in reported cases compared to 30 years ago. Although there is no known cause there are proven links to asthma and hay fever.
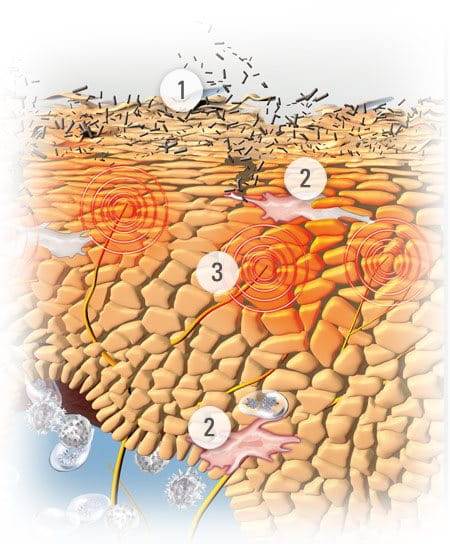
Sufferers experience dysfunctions of the skin barrier function and the immune system. The disease is characterised by two distinct phases. In a non-active (or “interval”) phase, skin is dry, irritable and may be slightly flaky. This dry or very dry condition is known as Xerosis . In active (or “flare-up”) phases, skin becomes infected, inflamed and itchy. While there is no known cure for Atopic Dermatitis, sufferers can help prolong the non-active periods, and help to reduce flare-ups with consistent skin care.
During an active phase, a sufferer would most commonly get a rash on his or her face, scalp, neck, décolletage, the insides of their knees and elbows, theirs hands, wrists and feet. These areas differ substantially in children and babies.


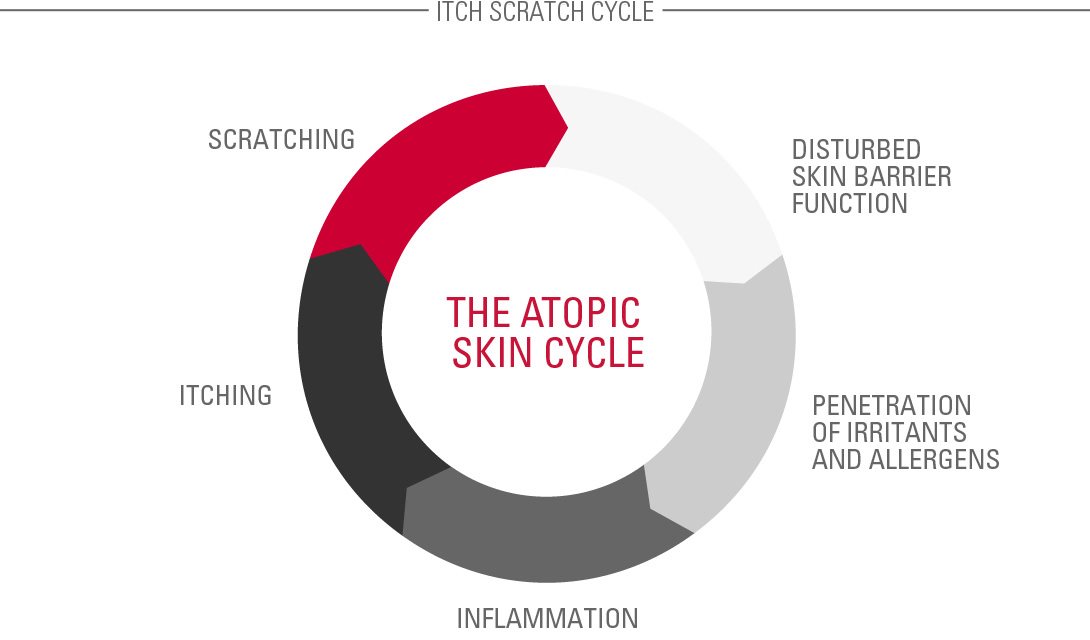
These rashes become itchy and inflamed and a vicious circle of scratching leads to further infection. Because atopic skin is so dry and itchy sufferers naturally scratch. This causes damage to the skin barrier, making underlying layers vulnerable to microorganisms and environmental pollution.
Flare-ups need to be controlled with anti-itch, anti-inflammatory and anti-bacterial dermatological treatments.
Atopic Dermatitis on the body can be aggravated by temperature so sufferers often have to limit the fabrics they wear, favouring soft cotton over wool or nylon. They may also suffer from sleep deprivation due to sweating and scratching.
Attention
If you are unsure about your symptoms seek the advice of a dermatologist.
Causes & Triggers
Potential causes and triggers of Atopic Dermatitis
Dermatologists have identified several causative and contributory factors.


For example:
- There appears to be a genetic link that connects Atopic Dermatitis, asthma and hay fever. If one or more parents have one or more of these conditions, their child’s risk of developing Atopic Dermatitis increases proportionately. If both parents have Atopic Dermatitis, there is a 60-80% chance that their child will inherit the disease.
- Links have been found between the environment someone lives in and their risk of developing the disease. Urban cities, where pollution is high, and cold climates are known to put people more at risk. In one study, comparing Jamaican children living in London with those living in Jamaica, there were twice as many cases in the London-based children.
- Mothers that give birth late into their child bearing years are more likely to have a child with Atopic Dermatitis than those that give birth younger.
Hereditary Atopic Dermatitis is characterised by a deficiency in natural moisturing factors (NMF) such as amino acids and a disturbance of the epidermal lipid metabolism.
Flare-ups can be triggered by the Atopic Skin Cycle whereby scratching creates a vicious circle of symptoms and reactions.
Contributing Factors
Further contributing factors


When Atopic Dermatitis affects the skin it is important to keep skin cool and irritation-free. Aggravating factors include:
- Clothes that make the body sweat, such as non-breathable nylon
- Clothes that are rough against irritated skin, such as wool
- Certain foods. These vary from person to person but common triggers include dairy products, nuts and shellfish
- Alcohol
- House mites, dust, pollen or other allergens
- Harsh washing detergents
- Formaldehyde
- Cigarette and cigar smoke
- Pollution
Stress and a lack of sleep can also make symptoms worse.
Read more about factors that influence skin.
Solutions
Alleviating the discomfort of Atopic Dermatitis in a flare-up
There is currently no cure for Atopic Dermatitis but symptoms in both active and non-active phases can be eased with consistent, effective skin care and appropriate medical treatment. However, even with the most stringent skin care routine, flare-ups do happen and sufferers need to find ways to alleviate the discomfort.
Emollients
Also called moisturisers, emollients help to keep skin supple and moist and reduce itchiness that can lead to a flare-up. These creams, lotions, bath additives and shower oils keep skin moisturised, which protects the surface from the damage caused by scratching.
Ingredients often found in emollients include:
- Omega-6-fatty acids: Evening Primrose Oil and Grape Seed Oil replenish skin’s natural protective barrier and soothe and nourish the skin.
- Licochalcone A (an extract of the licorice root). A natural anti-inflammatory and antioxidant, exclusive to Beiersdorf, that helps reduce redness and soothe inflammation.
Dermatological treatments
When flare-ups do occur, it is advisable to supplement the emollients with more active care. Products for flare-ups usually contain corticosteroids. These are known to be fast-reacting and effective at relieving inflammation and itching. However, they should not be applied on large areas of the skin over longer periods of time as their efficacy may decrease under prolonged use. For those reasons effective corticosteroids are prescription-only drugs.


Eucerin‘s AtoControl Acute Care Cream has skin caring properties that have been clinically proven to significantly improve the skin‘s appearance during flare-up phases. This caring skin solution helps reduce the use of hydrocortisone during flare-ups. Eucerin AtoControl Acute Care Cream is not a pharmaceutical product and is not meant to replace one.
Daily personal care for Atopic Dermatitis on the body
Everyone’s symptoms differ but there are a number of lifestyle changes that sufferer consistently say help them manage their Atopic Dermatitis.


For example:
- Keeping room temperatures cool but not cold. Sweating triggers irritation and itch.
- Putting creams and ointments in the fridge as cooled emollients offer additional itch relief.
- Keeping a diary of foods, drinks and potential environmental changes to see if any affect symptoms.
- Certain holiday destinations are thought to be more therapeutic than others. Good examples include the North Sea, Atlantic, Dead Sea, Mediterranean Sea and high mountain areas – although extreme cold must be avoided.
- Yoga and meditation help reduce stress, one of the triggers of flare-ups.
- When skin becomes itchy, it is better to pat rather than scratch. Both soothe skin but patting doesn’t damage the skin barrier.
- If the sufferer is a child, keep their nails short and smooth to minimise any damage they may cause by scratching.
- Try wearing cotton gloves at night to avoid scratching your body while sleep.
- Taking showers rather than baths and keeping the temperature below 32°. It can dehydrate skin to shower too frequently.
- Rather than rubbing wet skin with a towel, pat it almost dry, then apply cream or lotion directly after.
- Avoid aggressors like harsh body brushes or exfoliating gloves.
Attention
If you are unsure which management route to take please seek the advice of a doctor or dermatologist.
Our brand values

We deliver a holistic dermo-cosmetic approach to protect your skin, keep it healthy and radiant.

We work together with leading dermatologist and pharmacist partners around the world to create innovative and effective skincare products they can trust and recommend.

For over 100 years, we have dedicated ourselves to researching and innovating in the field of skin science. We believe in creating active ingredients and soothing formulas with high tolerability that work to help you live your life better each day.

